Questions for your Breast Surgeon:
- What are my surgical options?
- What surgery do you recommend for me?
- What is the difference in recovery?
- How do the “local recurrence” rates differ?
- Can you outline the possible complications of both surgeries?
- Should I do “Genetic Testing” before surgery?
Lumpectomy vs. Mastectomy surgery options
A Lumpectomy (followed by radiation) for early stage breast cancer is generally considered the optimal choice because it is less invasive and has the same cure rates as a mastectomy. At surgery, the breast cancer “lump” is removed with a margin of normal tissue around it. You are able to keep your breast with a lumpectomy, but you will likely benefit from a course of radiation to that breast to lessen the risk of developing a recurrence of cancer in the lumpectomy area of the breast in the future. It is important to note that some may not be good candidates for a lumpectomy.
A Mastectomy (usually without radiation) for early stage breast cancer is a more involved surgery especially if breast reconstruction is performed. It is important to understand that multiple surgeries are often needed by a plastic surgeon to ultimately achieve a symmetric cosmetic outcome. “Nipple-sparing” and “skin-sparing” mastectomy techniques can now achieve better cosmetic outcomes than in the past. One advantage is that you can generally avoid radiation for early-stage breast cancer. A mastectomy does not generally improve survival rates compared to lumpectomy for early-stage breast cancer.
Why is breast surgery a complex decision?
Every patient presents with a unique breast cancer situation. Your breast surgeon is the key person to understand what surgical options will serve you the best. Multiple cancer factors play into these options. These include the size of the tumor, the shape and form of the breast, whether there are multiple tumors in the same breast, and if the patient is a candidate for radiation therapy. This is a complex decision and recommendations may differ amongst surgeons. Most importantly, it is up to you to make a well-informed decision that suits you as a person and a patient.
Do I have time to decide what surgery is best?
This is a difficult time and one of information overload. You have plenty of time to learn more about your breast cancer and discuss your options with your breast surgeon. Taking a few weeks to make a decision has not been shown to have an effect on your cancer outcome. Early-stage breast cancer usually can be managed with either a lumpectomy followed by radiation or a mastectomy alone. There are distinct advantages and disadvantages to both approaches. When you are well educated about your options, you will be better prepared to work with your breast surgeon to decide what surgery is best for you.
“I feel pressured” to make a decision.
Your surgeon will review the details of your imaging, examine you, and possibly perform a breast and axillary ultrasound in the office. Afterward, he or she will provide you with surgical recommendations and discuss all of your options. During this discussion, you must focus on the information shared and ask key questions in order to make the best decisions. You will likely be asked to tentatively commit to a surgical decision so your surgeon can begin the process of scheduling your surgery. It is natural to feel pressured to make this important decision.
It’s important to note that you can always change your mind about your surgical decision. You will likely have one more office consultation before the surgery to review everything in more detail. This is also a time to ask more questions and share any reservations you may have.
Myths and Facts about surgery and early-stage cancer:
- A mastectomy does not reduce the need for chemotherapy
- Lumpectomy is an outpatient surgery
- It generally takes 3 to 6 weeks to schedule a mastectomy with reconstruction
- Genetic testing before surgery can sometimes alter your decisions
- Breast radiation after a lumpectomy usually takes 4 to 6 weeks
Does a mastectomy increase my odds of survival?
A mastectomy does not increase your odds of survival for early-stage breast cancer. This question has been studied in detail. If you have a lumpectomy and radiation, your chance of being alive ten years later is exactly the same as if you had a mastectomy without radiation. Survival is the most important cancer outcome we measure. It is the same for both treatment approaches for early-stage cancer.
There are a couple of caveats about “local recurrence” of cancer in the breast. A mastectomy for early-stage cancer removes about 90% of the breast tissue and leaves behind the skin of the breast in which cancer cells can grow in the future. The chance of cancer re-growing back in the area of a mastectomy is about 3% over 10 years. The chance of “local recurrence” after a lumpectomy and radiation is about 5 to 8% over 10 years. After a lumpectomy, women are screened with annual mammograms to quickly detect any recurrence or new breast cancers in the future. Mammographic screening is not needed after a mastectomy.
Why do some choose a mastectomy over a lumpectomy?
Most of the time this choice is a personal one for a variety of reasons. There are legitimate differences between the two surgical approaches involving recovery, side effects, complications, and costs. It is important to realize that everyone has different goals, unique personal situations, and their own reasons as to how they manage their health issues. “Patient autonomy” is essential to a great doctor-patient relationship. The more informed you become, the better decisions you will make for your own cancer situation. Don’t allow anyone on your treatment team to be dismissive of your own needs and desires.
Ask about BRCA Genetic testing before surgery.
You need to ask yourself this question, “If I have cancer and carry the BRCA mutation, would I change my mind about surgery and have both breasts removed to reduce my risks of having another new breast cancer in the future?” If the answer is yes or maybe, you should consider undergoing genetic testing before your recommended surgery. If the answer is no, then you can undergo testing after surgery.
If you qualify for genetic testing, the results can take about two weeks to be finalized. Be aware that waiting for these results can delay your surgical plans. Some women who qualify for BRCA genetic testing and are proven to have this broken gene may choose “risk-reducing,” bilateral (double) mastectomies. These agonizingly difficult decisions are made in consultation with your breast surgeon. Raise the question of genetic testing during your initial breast surgery consultation. If you do carry the mutation, you may choose a different surgery for treating your breast cancer. Only a small percentage of women harbor the BRCA mutation. The Breast Cancer School for Patients advocates identifying those at risk for the BRCA mutation before breast cancer surgery. Our video lesson on “BRCA Genetic Testing“ (here) outlines this topic in great detail.
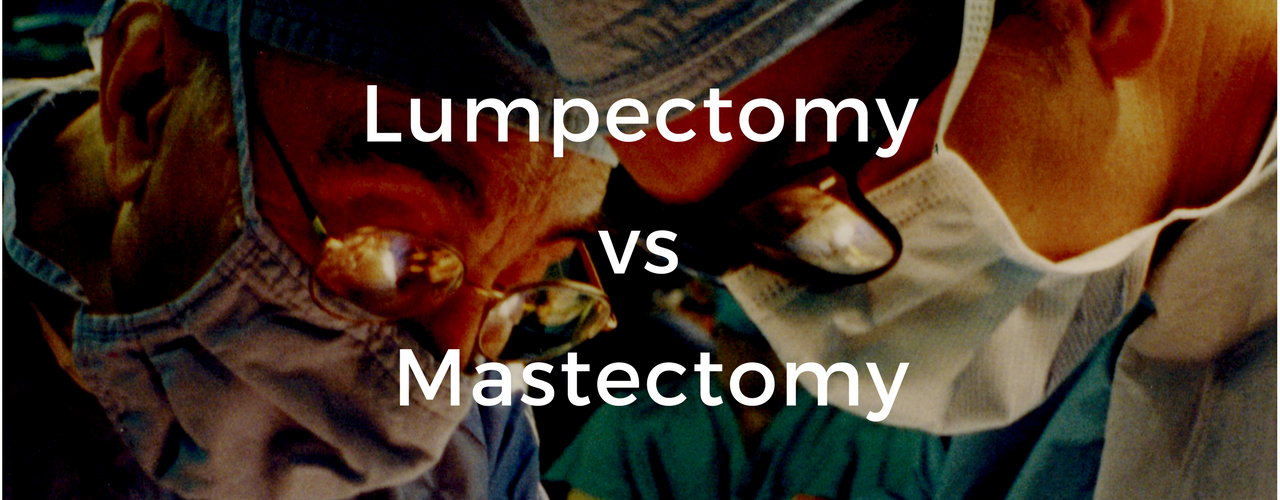
This “Option Grid” (here) is an excellent resource to learn about the differences between a lumpectomy and a mastectomy:
Patient-Friendly References:
Review their pages on “Lumpectomy” (here) and “Mastectomy” (here). There is excellent detail about all of your surgical options on this website. This site is created for patients by the American Society of Breast Surgeons.
This is a detailed outline (here) of treatment options for women with breast cancer, written specifically for patients. Choose the brochure that best reflects your own unique situation. The NCCN is a consortium of organizations and governmental agencies to promote quality breast cancer care.
This outline on “Breast Cancer: Surgical Options” (here) is a cutting-edge presentation of the differences between a lumpectomy and mastectomy. The Option Grid Collaborative is one of the largest developers of clinical decision aids. It is based at the Dartmouth Institute for Health Policy and Clinical Practice.
This excellent outline, “Breast Reconstruction after Mastectomy” (here) is a presentation of breast reconstruction options. The Option Grid Collaborative is one of the largest developers of clinical decision aids. It is based at the Dartmouth Institute for Health Policy and Clinical Practice.
More Detailed References:
This consensus statement (here) “Performance and Practice Guidelines for Lumpectomy” outlines indications and techniques associated with a lumpectomy. The American Society of Breast Surgeons is a leading organization of surgeons who treat diseases of the breast.
This consensus statement (here) “Breast Cancer Lumpectomy Margins” reviews recommendations for achieving adequate “margins” around cancer with a lumpectomy. The American Society of Breast Surgeons is a leading organization of surgeons who treat diseases of the breast.
This consensus statement (here) “Performance and Practice Guidelines for Mastectomy” outlines some of the indications and techniques associated with a mastectomy. The American Society of Breast Surgeons is a leading organization of surgeons who treat diseases of the breast.
If you want to get deep into the details, this free 200-page PDF document (here) has guidelines to help clinicians to make treatment recommendations about nearly all aspects of breast cancer. You can easily register (here) as a non-professional to get access and more information about breast cancer. The National Comprehensive Cancer Network is the leading organization in developing clinical guidelines.